Spring 2021 Issue |
|
EVMS HOPES Mental Health Clinic Addresses Local Health Disparities
By Aaliyah Joseph, BA and Dr. Stephanie Peglow, DO, MPH, FASAM, FAPA
Eastern Virginia Medical School
 |
| Aaliyah Joseph EVMS Student and HOPES Mental Health Clinic Coordinator |
Three years ago, I enrolled in a course entitled When Nightmare is Real: Trauma in Childhood and Adolescence, oblivious to the degree in which it would impact my life.
I learned about a three-year-old girl named “Tina” who not only witnessed the murder of her mother, but was brutally assaulted herself and left in a room with her mother’s dead body for 16 hours. Although she was able to live a relatively normal life after working with a psychiatrist, her early life experiences still impacted her negatively. I became fascinated with the brain, specifically its plasticity which plays a role in resilience and how trauma can shape one’s perception of and interaction with the world.
However, there are more contributing factors that led to my pursuit of becoming a psychiatrist. From witnessing people jumping in front of the train during my commutes to school in New York, to learning that my undergraduate institution’s library was “suicide-proofed” due to the number of students attempting suicide there, I realized that a significant number of people are suffering from mental illness and are doing so in silence.
Mental illness is a major public health issue. In fact, a 2016 Needs Assessment conducted by Norfolk Sentara Hospital and an EVMS fourth-year medical student (M4) Joshua Dellinger identified mental health as the most important health problem in the Norfolk region. The same assessment was readministered in 2019, and the results remained the same. The HOPES Mental Health Clinic was created by Joshua Dellinger and Dr. Stephanie Peglow in 2017 to address Norfolk’s dire need for mental health services.
The HOPES (Health Outreach Partnership of EVMS Students) Clinic is the first student-run clinic to be established in the state of Virginia and serves the uninsured and/or underinsured in Hampton Roads. The patient population we serve includes Spanish-speaking, homeless, and undocumented individuals. In addition to free mental health treatment, HOPES provides free primary care and other specialty care services such as dermatology, ophthalmology, and women’s health.
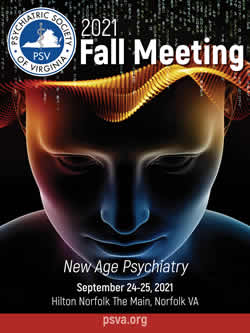
Attending Psychiatrist, Dr. Stephanie Peglow, discussing patient cases with Resident Psychiatrists Dr. Kelsey Johnson and Dr. Elizabeth Monter
Naturally, I signed up to volunteer for the Mental Health Clinic because it combined my two passions; addressing health disparities and serving as a mental health advocate. I shadowed the upper-class medical students and asked the attending any questions I had about the field of psychiatry. My favorite part of volunteering at HOPES is being surrounded by a group of medical students and physicians who are dedicated to serving disadvantaged populations, as well as participating in community outreach. For instance, I attended a re-entry fair at a local jail to inform individuals about the free mental health services that are available at HOPES upon their release. Later, I was appointed the Clinic Coordinator position for the Mental Health Clinic.
Aaliyah Joseph (left), Charmante Baucom (middle), and Ioaka Whilby (right) reviewing the clinic schedule
A typical shift at the HOPES Mental Health Clinic involves a team of M1-M4 students, two resident psychiatrists, and an attending psychiatrist; everything is team based. The M1s and M2s are responsible for writing the medical note, the M3s and M4s conduct the medical interview, the residents propose a treatment plan and teach, and the attending supervises. The Clinic Coordinator recruits volunteers, helps with scheduling patients, monitors patient load, coordinates clinic dates, and addresses any technical issues that may arise during clinic. Services we provide include diagnostic interviews, medication management and counseling services.
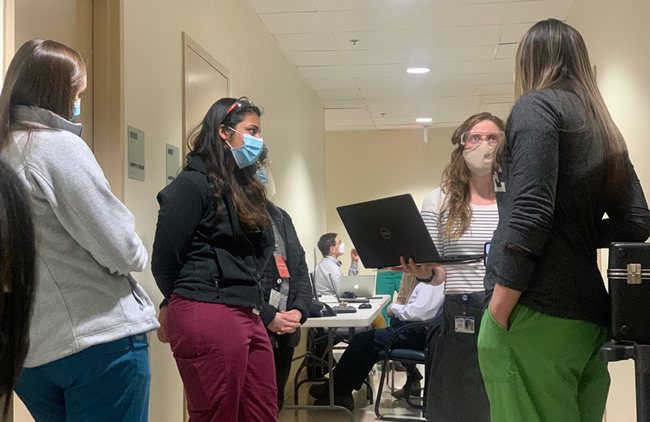
Nitasha Sharma, M4, and Morgan Shelton, M1, present patient case to resident and attending
When the COVID-19 pandemic started in March 2020, HOPES was forced to close its doors to patients, medical students, and physician volunteers. I transitioned the HOPES Mental Health Clinic to remote operation in an effort to avoid a break in the continuity of care for patients who already face tremendous barriers to accessing health services. We were the only specialty clinic to continue to accept new patients during this time. Through telemedicine, we’ve been able to connect more individuals to free mental health treatment. In addition, there has been a significant increase in the number of patients attending their scheduled appointments. I postulate this increase is due to transportation no longer being a barrier to accessing healthcare.
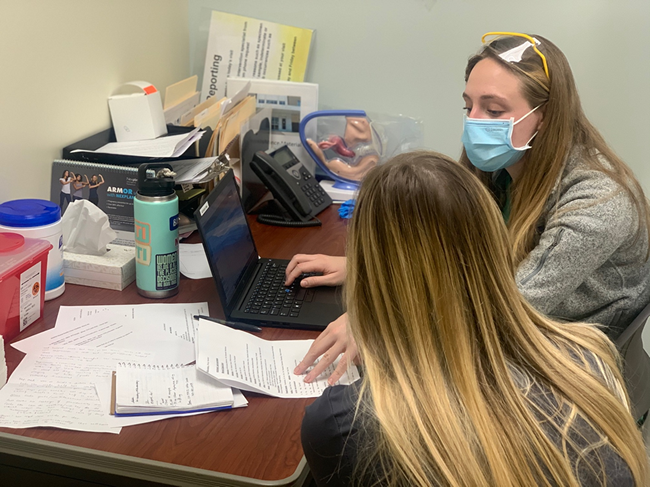
Emily Breeding, M3, and Kelly Bryant, M1, reviewing medical interview findings
Lastly, telemedicine has enabled us to connect with patients experiencing a severe mental health crisis. For instance, we had one patient with several existing psychiatric conditions that were exacerbated due to the pandemic negatively impacting their life. During their appointment, we found that they were actively suicidal. Fortunately, we were able to intervene and get them the help that they needed. Since I started volunteering at HOPES in 2019, I never came across a suicidal patient. Given the mental state of that patient at the time, I sometimes wonder if they would have made their appointment that day if we hosted the clinic in-person rather than virtually. After the event, we received updates that the patient’s symptoms improved. They have transitioned to a higher level of care with our help, and they were very thankful for HOPES.

Aaliyah Joseph volunteering at Street Health Clinic
Community outreach is an important component of the HOPES Mental Health Clinic and we frequently collaborate with other organizations to connect individuals to free mental health treatment. Currently, we have a partnership with Street Health, another EVMS student-run free clinic that serves the homeless population in Norfolk and provides free primary care. Any patient at Street Health who is in need of mental healthcare is referred to our clinic and I volunteer at Street Health to assist in making that transition of care as smooth as possible.
In addition, we have another partnership with the Norfolk Sheriff’s Office. I established a mental health education program where EVMS students lead classes on topics such as anger management, addiction and recovery, and identifying mental illness under the supervision of a mental health professional. The purpose of this program is to increase the mental health literacy of the local incarcerated population and connect uninsured and/or underinsured individuals to HOPES upon their release.
Lastly, we recently partnered with Intensive Community Outreach Services (ICOS) to provide crisis stabilization, family counseling, and mental health courses to help individuals function independently in society. In the future, I hope to create a mobile clinic where we can “meet people where they are” to provide mental health treatment.
In conclusion, the HOPES Mental Health Clinic provides a much-needed service to Hampton Roads residents. Additionally, it provides students with a unique learning experience in Outpatient Psychiatry. We’ve received feedback that the HOPES Clinic was instrumental in some students’ residency choice of Psychiatry. I’m confident that the knowledge and experiences I gained from volunteering at the HOPES Mental Health Clinic will help me become an amazing psychiatrist one day.
If you are interested in volunteering at our clinic, please contact me at [email protected]. We currently offer in-person and virtual volunteer opportunities. EVMS covers malpractice for volunteers, however, a Virginia License is a requirement. We will take care of the rest!
YOUR NEWSLETTER IS NOW AVAILABLE ON YOUR SMARTPHONE AND TABLET!
JOIN PSV TODAY!
PLAN NOW!
PSV 2021
FALL MEETING
September 24-25, 2021
Hilton
Norfolk The Main
Norfolk, VA
APA Find a Psychiatrist
Are you accepting new patients?
Opt into APA’s Find A Psychiatrist database. To view the functionality or opt-in,
CLICK HERE
FYI: A link for this option has been added to the PSV website. Select the About button and then Find a Psychiatrist from the drop down.